Covid variant competition and a longer-term strategy
How do new Covid strains replace older ones? A simple model provides some answers:
The model consists of three rules:
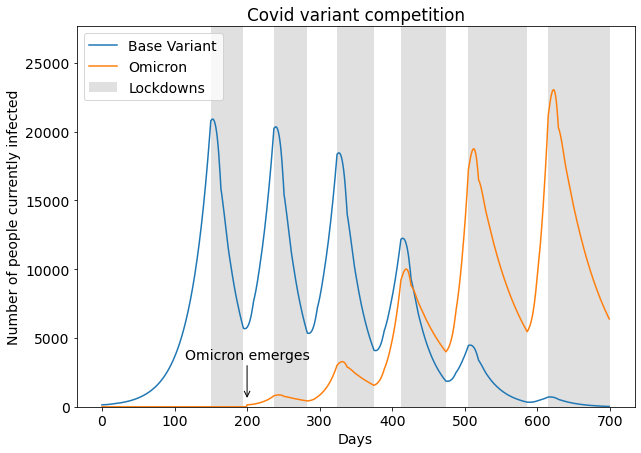
- At the beginning only the base variant exists, until on day 200 the Omicron variant appears.
- Each base variant infection causes 1.25 follow-up infections. Each Omicron infection causes 1.40 follow-up infections.
- A lockdown starts when the number of sick people reaches 20000. This results in a reduction of new infections by 36%. The lockdown ends when the number of sick people falls below 6000 again.
This might be the world's worst Covid model, but it gets one thing right: the competition between variants. It shows the dynamic:
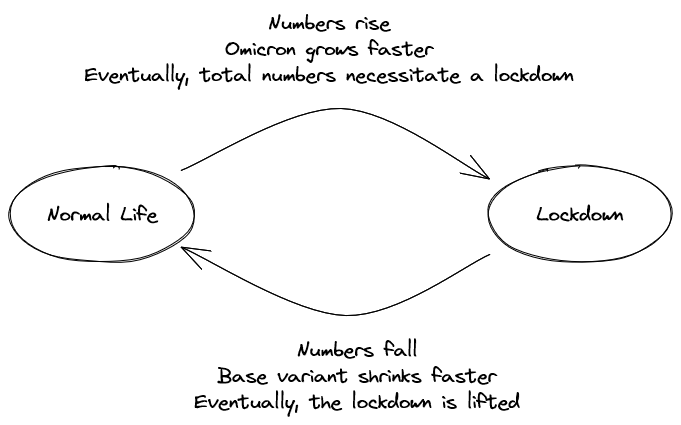
Earlier variants vanish due to the stronger human interventions required to keep the newer variants in check. We decide on preventive measures based on total numbers, not per-variant details. More infectious strains require longer, more frequent, or more stringent lockdowns. These measures hit older variants harder, which makes them recede.1
At some point we might not be able to enact strict enough countermeasures to prevent newly evolved strains from spreading. Arguably, this already applies to Omicron. If not, new variants will continue to emerge. Our lukewarm vaccination efforts exacerbate this issue by applying evolutionary pressure on the virus. Vaccination rates are high enough to stop earlier strains, but low enough to allow the spread of more infectious, more vaccination-resistant variants. Thus, we should expect to see more problematic strains in the future.
Where does this leave us? Covid is on track to become endemic, so everyone will get infected eventually. The big question is how to manage this process without overwhelmed hospitals, and ideally without endless lockdowns. Vaccination is a key ingredient, since it reduces hospitalization and death rates tenfold. A 100%-vaccinated society could support ten times more infections at the same time.2 During Corona peaks, masks, social distancing, and lockdowns help to remove pressure from hospitals. Outside of peak seasons, a relaxed approach is probably best.
1 Does this argument still hold despite the lower hospitalization rates of Omicron patients? It does: avoiding overwhelmed hospitals still requires strict Omicron countermeasures, just at a higher number of infected people.
2 Compared to an unvaccinated society. Countries with a 65–75% vaccination rate can afford 3–4 times the infections as before vaccination campaigns. The comparison of Covid numbers of winter 2020/2021 and winter 2021/2022 supports this.
Comments